What Are Autoimmune Conditions & How Do They Work?
Share
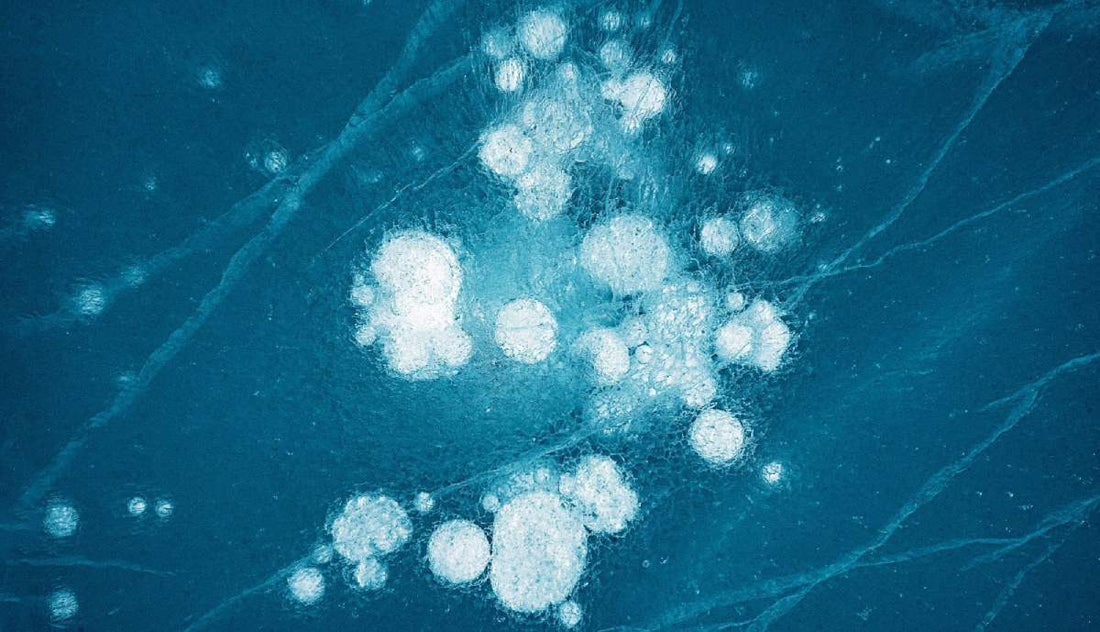
Autoimmune conditions affect millions of people worldwide, with women being disproportionately impacted. But what is an autoimmune disease? In simple terms, it is a condition where the immune system, designed to protect us, mistakenly attacks healthy cells, tissues, or organs. This blog will break down the science behind autoimmune diseases, outline a list of autoimmune diseases and symptoms, and explain the latest treatment and management strategies.
Immune System 101 … Friend or Foe?
How a Healthy Immune System Protects Us
The immune system acts as the body's defense force, identifying and neutralizing harmful invaders like bacteria, viruses, and toxins. It does this through white blood cells, antibodies, and chemical messengers called cytokines. When functioning correctly, the immune system keeps us healthy and prevents infections.
Autoimmunity Defined: When Defense Turns to Attack
What are autoimmune diseases exactly? Autoimmune diseases occur when the immune system loses its ability to distinguish between self and non-self. Instead of targeting pathogens, it creates autoantibodies and activates T-cells that attack the body's own tissues. This can lead to inflammation, tissue damage, and loss of function in affected organs.
Key Players: Antibodies, T‑Cells, and Cytokines
-
Antibodies: Y-shaped proteins that typically target pathogens but may attack healthy tissue in autoimmunity.
-
T-Cells: White blood cells that directly kill infected or abnormal cells but can become misdirected in autoimmune conditions.
-
Cytokines: Chemical messengers that regulate immune responses, often involved in driving chronic inflammation seen in autoimmune diseases.
What Causes Autoimmune Diseases?
Genetics & Family History
A significant portion of autoimmune risk comes from genes. Specific gene variants can make someone more susceptible to autoimmune diseases. For example, the HLA (human leukocyte antigen) genes play a key role in immune system regulation and are commonly linked to autoimmune conditions.
Environmental Triggers (Infections, Toxins)
Factors like viral or bacterial infections, exposure to chemicals, or heavy metals can initiate or exacerbate autoimmune disease symptoms. Researchers believe environmental triggers often interact with genetic predispositions.
Hormonal & Gender Factors (Why Women Are Affected More)
Women are up to three times more likely to develop autoimmune conditions than men. Hormonal differences, especially fluctuations in estrogen and progesterone, influence immune system activity. Autoimmune flare-ups often occur during pregnancy, postpartum periods, or menopause.
The Gut–Immune Connection
The gut microbiome plays a critical role in immune regulation. Imbalances in gut bacteria, known as dysbiosis, can contribute to the causes of autoimmune disease. This gut–immune relationship is a major focus in current autoimmune research.
Common Autoimmune Conditions Explained
Rheumatoid Arthritis (RA)
A systemic autoimmune disease where the immune system attacks joint linings, causing pain, swelling, and eventual joint damage.
Systemic Lupus Erythematosus (SLE)
Known simply as lupus, this disease affects multiple organ systems, including skin, joints, kidneys, and the heart. SLE presents with a variety of symptoms and is notoriously difficult to diagnose.
Type 1 Diabetes
In type 1 diabetes, the immune system destroys insulin-producing cells in the pancreas, leading to high blood sugar levels. It often develops in childhood but can occur at any age.
Hashimoto’s & Graves’ Thyroid Disease
Both affect thyroid function:
-
Hashimoto’s disease causes hypothyroidism, slowing metabolism.
-
Graves’ disease leads to hyperthyroidism, speeding up metabolism.
Multiple Sclerosis (MS)
An autoimmune condition where the immune system attacks the protective covering of nerves, leading to muscle weakness, coordination problems, and cognitive issues.
Psoriasis & Inflammatory Bowel Disease (IBD)
-
Psoriasis: A skin disorder marked by red, scaly patches.
-
IBD: Includes Crohn’s disease and ulcerative colitis, both of which inflame the digestive tract.
Signs & Symptoms—When to Suspect Autoimmunity
Systemic vs. Organ-Specific Indicators
Some autoimmune conditions affect specific organs, while others have widespread impact. Examples include:
-
Organ-specific: Hashimoto’s thyroiditis, Type 1 diabetes.
-
Systemic: Lupus, RA.
Flare-Ups and Remission Cycles
Many autoimmune diseases feature cycles of worsening symptoms (flares) followed by periods of improvement (remission). Recognizing patterns can help in management.
Overlapping Symptoms & Misdiagnosis Risks
Symptoms such as fatigue, joint pain, and skin rashes overlap with many other conditions. This often leads to delayed diagnosis or misdiagnosis, underscoring the importance of working with experienced specialists.
Diagnostic Journey
Blood Tests: ANA, ESR, CRP & Specific Antibodies
-
ANA (Antinuclear Antibody): Often positive in lupus and other systemic autoimmune diseases.
-
ESR (Erythrocyte Sedimentation Rate) and CRP (C-Reactive Protein): Markers of inflammation.
-
Specific Antibodies: Anti-dsDNA, rheumatoid factor, anti-CCP, and others help pinpoint the exact condition.
Imaging & Biopsy Procedures
X-rays, MRIs, and ultrasounds can reveal tissue and organ damage. Biopsies may be needed to confirm diagnoses, particularly in conditions like lupus or vasculitis.
Working with Rheumatologists & Specialists
Diagnosing and treating autoimmune conditions usually requires a team, including rheumatologists, endocrinologists, neurologists, and gastroenterologists.
Treatment & Management Options
Conventional Therapies (Steroids, DMARDs, Biologics)
-
Steroids reduce inflammation but have side effects with long-term use.
-
DMARDs (Disease-Modifying Antirheumatic Drugs) slow disease progression.
-
Biologic therapies target specific immune pathways and are increasingly common in treating autoimmune disease.
Lifestyle & Diet Strategies (Anti-Inflammatory Eating)
Anti-inflammatory diets rich in omega-3 fatty acids, antioxidants, and fiber can support immune balance. Avoiding processed foods and sugars is often recommended.
Stress Management & Sleep Hygiene
Chronic stress and poor sleep exacerbate autoimmune symptoms. Techniques like meditation, yoga, and cognitive behavioral therapy can help manage stress effectively.
Complementary Approaches (Supplements, Mind-Body)
Supplements such as vitamin D, omega-3s, and probiotics support immune regulation. Mind-body practices like acupuncture and tai chi may also provide relief, though evidence varies.
Living Well with an Autoimmune Condition
Flare Prevention Tips
-
Maintain consistent medication schedules.
-
Follow a tailored diet.
-
Avoid known environmental triggers.
Building a Support Network
Support groups, whether in-person or online, can be vital for mental health and treatment adherence.
Monitoring & Adjusting Treatment Plans
Autoimmune disease treatment is rarely static. Regular check-ups and lab work help fine-tune medication doses and identify potential side effects early.
Future of Autoimmune Research
Precision Medicine & Genetic Insights
Researchers are exploring genetic markers that predict disease risk and treatment response, paving the way for more personalized care.
Microbiome-Targeted Therapies
Emerging treatments aim to restore gut health to modulate immune responses, offering new hope for autoimmune conditions.
Emerging Biologic & Cell-Based Treatments
Advanced therapies, including stem cell transplants and new biologic drugs, are being tested to provide more effective and longer-lasting relief.
Frequently Asked Questions (FAQ)
What exactly triggers an autoimmune disease?
While the causes of autoimmune disease are not fully understood, a combination of genetic predisposition, environmental triggers, and hormonal factors likely plays a role.
Are autoimmune diseases curable?
Most autoimmune diseases are chronic but manageable. While some people achieve remission, there is currently no universal cure.
Why are women more prone to autoimmunity?
Hormonal fluctuations and genetic factors unique to females contribute to higher rates of autoimmune conditions in women.
How are autoimmune diseases diagnosed?
Through a combination of symptom assessment, blood tests, imaging, and specialist evaluations.
What is the difference between autoimmune and inflammatory diseases?
All autoimmune diseases are inflammatory, but not all inflammatory diseases are autoimmune. Inflammation can be triggered by infections, injuries, or other non-autoimmune processes.
Can autoimmune disease kill you? In severe, untreated cases, complications from organ damage or infections can be life-threatening. However, with proper diagnosis and management, many people live long, healthy lives with an autoimmune condition.
For more in-depth articles about mental health, immune system balance, and science-backed supplements for women, explore our blog or contact our wellness experts today.
